Expect more unplanned summer ER closures in rural Ontario, experts say

Unplanned emergency department closures are expected to continue through the summer in rural and northern communities in Ontario, according to some of the people responsible for helping to keep the doors open.
While the impact of COVID-19 on patient volumes and staff absences has lessened, temporary ER closures continue at hospitals across the province and stakeholders say the province needs to provide more than just short-term solutions.
"I can tell you that in Ontario every week there is an unplanned closure," said Dr. Alan Drummond, an emergency physician at the Perth and Smiths Falls District Hospital in Lanark County.
Drummond — a member of the Canadian Association of Emergency Physicians — underscored that prior to 2022, Ontario hadn't had an unplanned ER closure since 2006.
"And now they are routine and they are totally unnecessary," he said. "It's unacceptable."
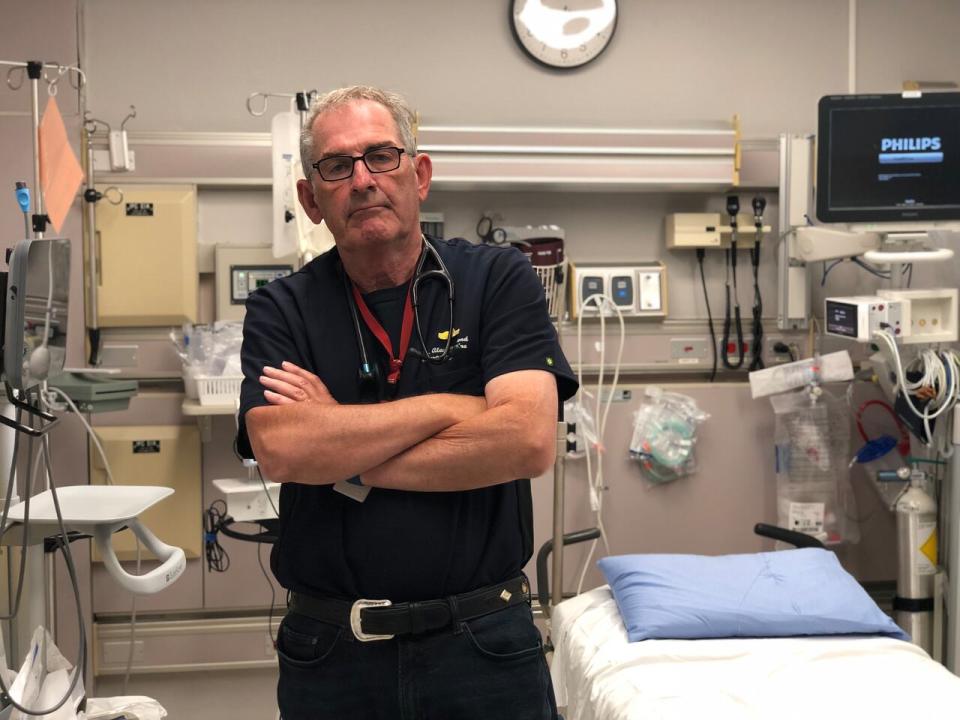
Dr. Alan Drummond with the Canadian Association of Emergency Physicians says there's one unplanned ED closure now each week in Ontario, when there used to be none prior to 2022. 'That's unacceptable,' he says. (Provided by Alan Drummond)
In Lanark County, the Almonte General Hospital, about 50 km west of Ottawa, has suffered a number of temporary ER closures over a nursing shortage, said Drummond. Patients can drive to other hospitals in the county, but Drummond says it causes a ripple effect.
"And that is always disconcerting and runs the risk of impacting neighbouring emergency departments and certainly undermining the confidence of people that live there."
This summer, as hospital staff begin much-needed vacations, covering off those absences will be challenging, he said.

Tim Vine, CEO of the North Shore Health Network says some 60 per cent of physician shifts are backfilled by temporary 'locum' doctors to keep the three hospitals in his region open on the north shore of Lake Huron. (Melanie Kubatlija)
Reliant on temporary doctors
The province has renewed the temporary locum program this spring for another six months, providing temporary doctors (called "locums") to fill in at ERs in rural and northern hospitals avoid temporary ER closures.
But Tim Vine, the CEO of the North Shore Health Network along the shore of Lake Huron between Sudbury and Sault Ste. Marie, Ont., says the temporary nature of the program means hospitals remain vulnerable.
Vine told CBC some 50 to 60 per cent of physician shifts are backfilled by locums, and the six months of funding doesn't help recruit doctors to stay long term.
"It does create a vulnerability for us because we have become so reliant on locums," said Vine.
As for nurses, Vine says recruitment has improved as efforts to train more workers begin to bear fruit. Pay for nurses has also increased since last year's arbitrator's decision to award nurses an 11 per cent increase over two years.
But the reliance on agency nurses adds a strain to hospital budgets.
Vine said his hospitals will spend up to $900,000 this year on agencies. It's down from the million spent last year.
"So to spend almost $1 million on agency nurses is a financial strain for us and is a cost to the health system," said Vine, noting it's twice the cost of what it should normally cost for nurses, with no improvement to access, and adds the burden of constant retraining.
Retention of staff nurses also remains a big problem, Vine said.
Provincial programs to ERs open
The province has been providing some investments to keep ERs open, including the physician locum program and a new consult program for doctors in small facilities who need timely, and sometimes ongoing help from specialists.
Emergency physician Dr. Howard Ovens, chief medical strategy officer at Sinai Health System, has been involved in the province's efforts as chair of the emergency services advisory committee to the province, and physician lead for Ontario Health's new program in provincial emergency services.
He told CBC the consult program, called "ED Peer to Peer" involves more than two dozen specialists who understand the resource problems for rural hospitals, and has proven popular for some locations.
It began as a pilot, but has since been "expanded," according to Ontario's Health Ministry spokesperson Hannah Jensen.
The locum program, however, has been a temporary fix, requiring renewal every six months since it began last year.
"There remains a risk of closure in some communities, generally more frequently related to nurse staffing than physician staffing," wrote Ovens in an email, and said through his work with Ontario Health, they are working hard to keep emergency departments open and the great majority of the time are successful.
But Drummond says for every ER that closes, there are 10 near misses. He says the locum program's six-month lifespan doesn't help long-term planning. This year it was renewed the same month it was set to expire.
"Why is it that we're waiting till the very last minute to announce funding and leaving hospitals in a situation where they're scrambling to guarantee staffing," said Drummond.
Vine said the last minute short-term funding for locums means they're not able to use that money to recruit a physician to stay, and so they're caught in a position where they've become dependent more and more on planning through crisis.
"This program is great to keep the lights on, but it doesn't allow for that future planning."


