'Nothing helped.' 2 Fredericton women endure long, painful wait for endometriosis surgery
If an animal in pain comes to the veterinary clinic where Jessica Grant and Mackenzie Ashby work — if it's bleeding or unable to eat — they exhaust all options to provide care, even as pain radiates through their own bodies, as medication makes their bones feel like they're filled with glass, and they struggle with depression.
Grant, 27, and Ashby, 37, work together as veterinary technicians in Fredericton. To watch animals receive better, faster health care than they do makes them feel less than human, like the butt of a cruel joke.
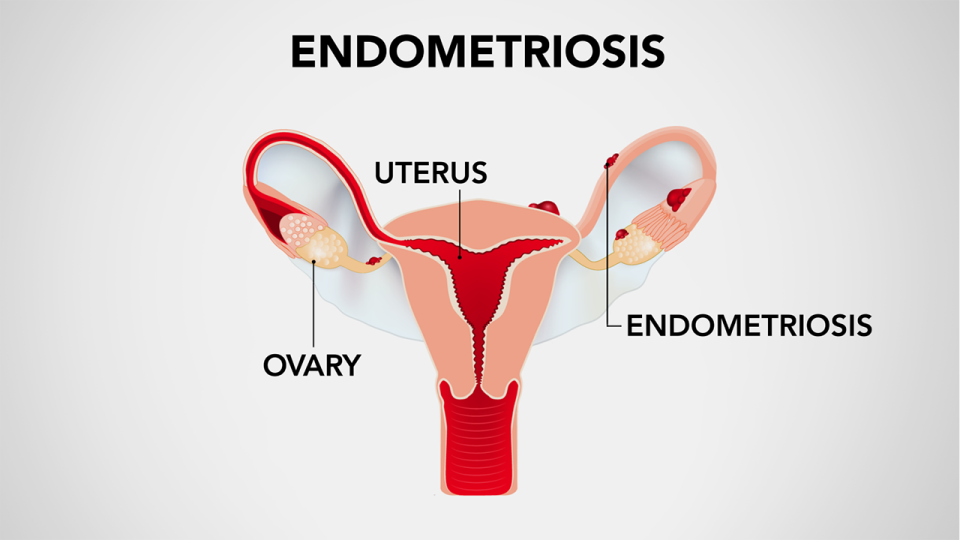
Both have endometriosis, a disease that occurs when cells similar to the lining of the uterus implant abnormally outside the uterus and form lesions, cysts and other growths, often causing heavy bleeding, severe pelvic pain and numerous other challenges.
Endometriosis has no cure, but excision surgery to remove the lesions is considered the gold standard for improving quality of life.
That sounds simple, but Grant and Ashby describe years of struggling to get access to care, from doctors telling them that period pain is normal and denying them hysterectomies to a long wait-list for surgery.

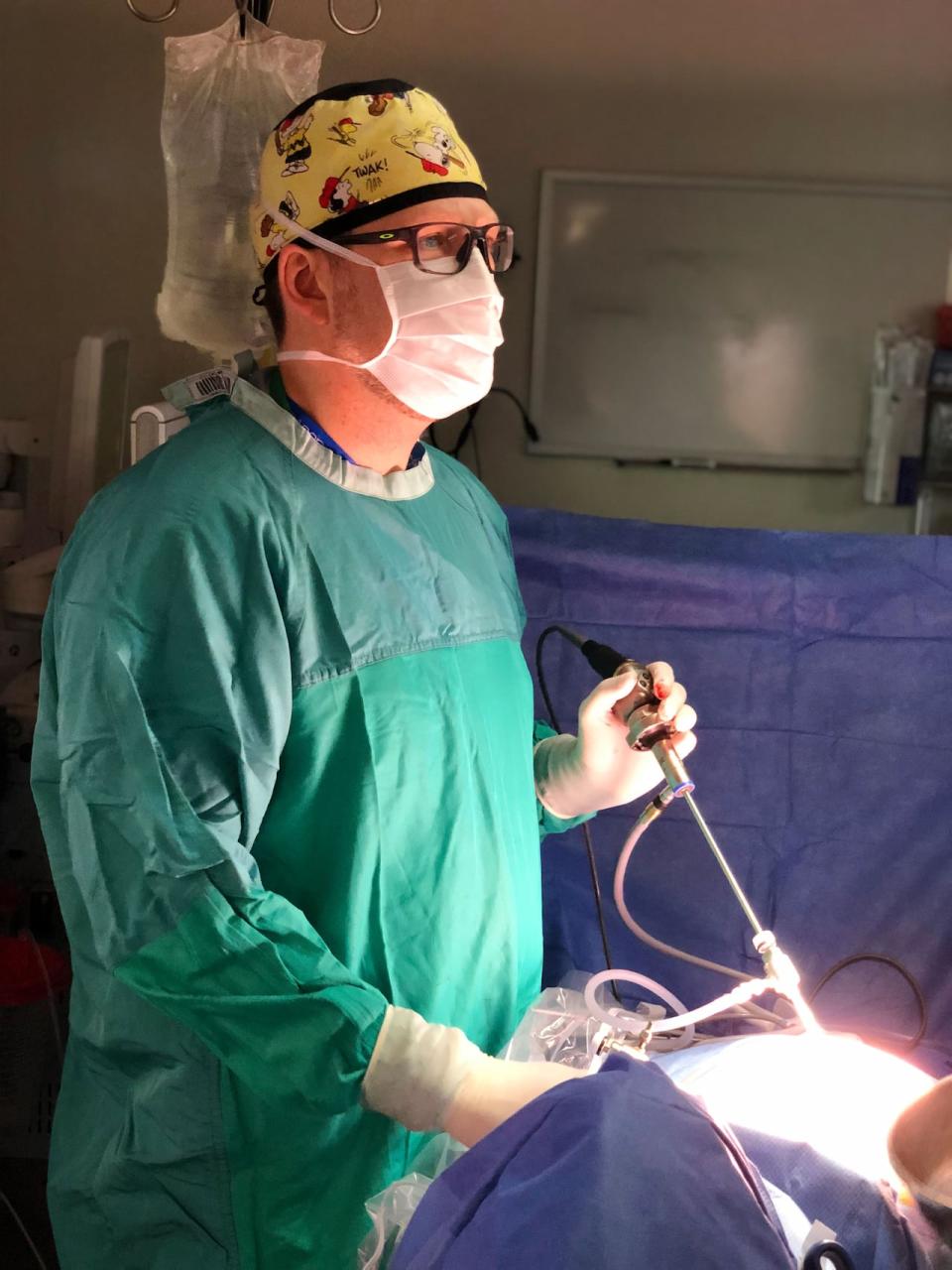
Grant and Ashby are now patients of Dr. Craig Morton, a gynecologist and endometriosis specialist in Saint John.
He says he receives two-and-a-half OR days per month and has a surgery wait-list of 12-24 months.
Morton said in an ideal world, he would have four to six days per month but there's a "huge backlog" of surgeries across the entire province.
WATCH | 'We need to stop telling women it's in their heads':
After returning from a fellowship in Calgary last May, where he received more specialized training for endometriosis surgeries, Morton said he has received an increase in referrals.
"It fundamentally has changed my practice and I think has been a positive thing for patients in New Brunswick," he said in an interview.
Grant was diagnosed with endometriosis in 2019 after years of pain so severe it sent her to the ER more than once, where she said she was told she had urinary tract infections.
"The last time I had gone it was to the point where I was calling into work, I was in so much pain. I was in the fetal position every single day. Nothing helped, no medications helped," she said.
Finally, after an 11-hour wait at the ER, an ultrasound revealed two large endometriomas, or cysts filled with blood, on her ovaries. She received a referral to a gynecologist, who put her on a medication that effectively put her body through menopause.
Grant was placed on Morton's surgery wait-list in July 2023 and still does not have a surgery date. She takes 14 pills a day, including four different pain medications, and recently has had breakthrough bleeding.
Her quality of life is terrible and, with no clear end in sight, Grant said she struggles with depression.
"I'm definitely in and out of depression and constantly thinking it would be better to be dead than to be on the planet," she said.
When her surgery finally does happen, Grant will have a hysterectomy.
Ashby is also planning to get a hysterectomy when she undergoes surgery. She, too, is waiting for a surgery date.
Growing up, Ashby said she was repeatedly told her period pain was normal. When she was in college, the pain was so severe she ended up going to the ER.
After a referral to a gynecologist and a lengthy wait, Ashby was diagnosed with endometriosis at the age of 24. She was put into medically-induced menopause and for six months suffered from hot flashes, joint pain and hormonal disruption.
Her doctor told her she should have a baby to relieve the symptoms.
That's an old adage, said Grant, that's both dismissive and unhelpful. Even if she wanted one, even if she could conceive, wouldn't the pain return after she had a child?
"You'll always be in pain," her doctor told her.

Ashby spent the next several years dealing with a heavy menstrual cycle. More ER visits. More medication. Pain when defecating, pain during sexual intercourse. Worsening depression.
Finally, in 2019, after her endometriosis had advanced, Ashby came up with the money to drive to Ottawa for excision surgery, since it was not available in New Brunswick at the time.
Ashby said the notes for the three-hour surgery said her disease was severe.
Today, she is on her third round of medically-induced menopause. Her endometriosis has returned in full force.
Over the past year, she said she's been in and out of the hospital for malnutrition and dehydration because she can't eat. A colonoscopy revealed her colon is adhered to one of her ovaries. She's lost 70 pounds and continues to lose weight.
"I'm looking outside of the country [for surgery] at this point," she said, adding that would cost her $17-30,000.
Ashby said she and her general practitioner both worry that if her condition worsens, her body will not be able to withstand the endometriosis surgery and that, eventually, malnutrition could lead to loss of life.
Ashby said she's emailed Morton about these new health issues and he said he's doing everything he can, but at the end of the day, he has a long patient list and can't make any guarantees.
"I can't blame him," Ashby said. "He's not making these policies, he's not doing anything wrong. He just can't get OR time."
Dr. Patricia Bryden, co-leader of surgical services for Horizon Health Network, said in a statement that allocation of OR time is patient-focused and based on overall wait-lists and historical data for higher acuity surgeries.
"As such, some surgeons and surgical specialities have more OR time than others," the statement said.
Morton said time in the OR is disrupted by nursing staff shortages, a lack of hospital beds for patients to recover from surgery and anesthesia shortages.
"It's frustrating for everybody involved," he said.
If you or someone you know is struggling, here's where to get help:


