Signs of Alzheimer’s were everywhere. Then his brain improved
Editor’s note: CNN Chief Medical Correspondent Dr. Sanjay Gupta’s documentary“The Last Alzheimer’s Patient” streams June 18 on MAX as part of “The Whole Story With Anderson Cooper.”
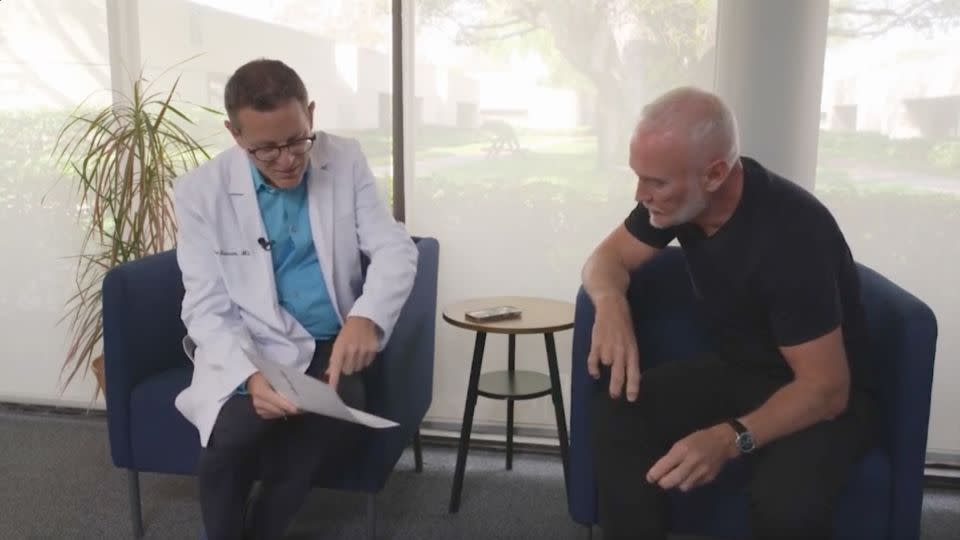
Preventive neurologist Dr Richard Isaacson stared at the numbers on the fax in astonishment. Blood biomarkers of telltale signs of early Alzheimer’s disease in the brain of his patient, 55-year-old entrepreneur Simon Nicholls, had all but disappeared in a mere 14 months.
“I had to catch my breath. It was a complete shock: The blood tests on his brain had normalized,” said Isaacson, director of research at the Institute for Neurodegenerative Diseases in Boca Raton, Florida.
Was this stunning result the work of some new miracle drug designed to combat dementia? Not at all. This is a story of old-fashioned grit and determination.
“Simon was on a mission, as if the Grim Reaper was peering over his shoulder. He was going to kick ass and take names,” Isaacson said.
Nicholls reduced his risk of developing Alzheimer’s via lifestyle changes recommended by Isaacson, including diet, exercise, reducing stress and optimizing sleep, along with a few strategically chosen supplements and medications prescribed by his cardiologist.
“I was very worried,” Nicholls told CNN Chief Medical Correspondent Dr. Sanjay Gupta in his new documentary, “The Last Alzheimer’s Patient,” which is airing on “The Whole Story with Anderson Cooper.”
“I have a 3-year-old son and an 8-year-old son. It’s really important for me, as I get older, to try and be there for them in the future,” he said. “There are many [changes] in lifestyle you can do to hopefully push the disease backwards and give yourself more time, which is all we need until we find a cure.”

Unlucky genes
When it came to genetics and dementia, Nicholls had drawn the short straw. He carried two copies of the APOE4 gene, one from each parent, which may increase the risk of developing Alzheimer’s at least tenfold.
“Sadly, my mum passed away from what we think is Alzheimer’s in her 70s,” Nicholls said. “For the last 10 years of her life, she just sat in a chair, rocking, while on about 14 medications. I’d much rather have a longer health span and then just go quickly.”
Not everyone with one or even two copies of APOE4 develops Alzheimer’s, however, creating a tantalizing opportunity. Can a person diminish their genetic risk for Alzheimer’s via lifestyle and various medical interventions, especially if started early, before too much damage is done?
Isaacson, who also has a family history of Alzheimer’s, believes the answer is yes. He began the first US clinic devoted to Alzheimer’s prevention in New York City in 2013 before moving his program to Florida in 2021. His research has shown that following a dozen or more lifestyle interventions, when practiced 60% or more of the time, can improve cognitive function, especially in women.

Today, scientists around the world are also investigating the impact on cognition of such lifestyle changes as a healthy plant-based diet, stress reduction, strength training, aerobic exercise and quality sleep habits — behaviors that Isaacson and his team outlined in a recent review published in Nature.
“I don’t use the term ‘reverse.’ I don’t know what reverse means when it comes to the field of Alzheimer’s,” Isaacson said. “But the results we’ve seen with Simon and some other patients in our research are extremely exciting.”
How the heart and the brain are intertwined
Alzheimer’s isn’t the only pathway to a life of dwindling memory and the inability to think, plan and interact with loved ones.
Vascular dementia, the second most common type of dementia after Alzheimer’s disease, can be caused by atherosclerosis, a buildup of plaque in the arteries that can lead to heart attacks, stroke, blood clots and more, all of which can further damage the body and brain.
Poor hearts and their consequences can run rampant in a family over generations, a fact Nicholls knew all too well.
“My whole family had endless heart attacks, resulting in my grandfather on my mother’s side dying around age 50,” he said. “My mother had three heart attacks, the first at age 50, then a triple bypass before she went on to develop dementia.”
Carrying an APOE4 gene further increases the risk for heart disease as well as dementia, experts say.
“My sister had three heart attacks, and when I was 40, I was told that I had atherosclerosis, with a ridiculously massive coronary artery calcium score of like 1,500 and occlusions in about 96% of my arteries.” A normal coronary artery calcium score is zero.
For a man in the prime of his life, the news was crushing. Doctors tried to use lifestyle changes and statins to reverse the plaque buildup but finally resorted to surgery, opening three of Nicholls’ arteries with stents. He also began using an injectable drug called evolocumab, designed to boost the liver’s ability to remove “bad” low-density lipoprotein, or LDL, from the body.
‘It was time to turn to my brain’
Slowly, Nicholls’ heart condition began to improve, but the bad news didn’t end there. A brain scan found telltale signs of vascular damage in Nicholls’ brain, which occurs when the tiniest blood vessels are starved of oxygen.
“The doctors said I had too many white matter lesions. I told myself that since I now had my heart more or less under control, it was time to turn to my brain,” Nicholls said.
In January 2023, Nicholls became participant No. 34 in a novel clinical trial at Isaacson’s Florida center. The trial is designed to uncover cognitive risk factors and counter them with a personalized plan of attack. (Full disclosure: I am participant No. 20 in the same trial; you can read about my experience here.)
“The overall goal of the study is democratize access to preventive neurology care by eventually using at-home blood testing to cost-effectively reach the most people,” Isaacson said.
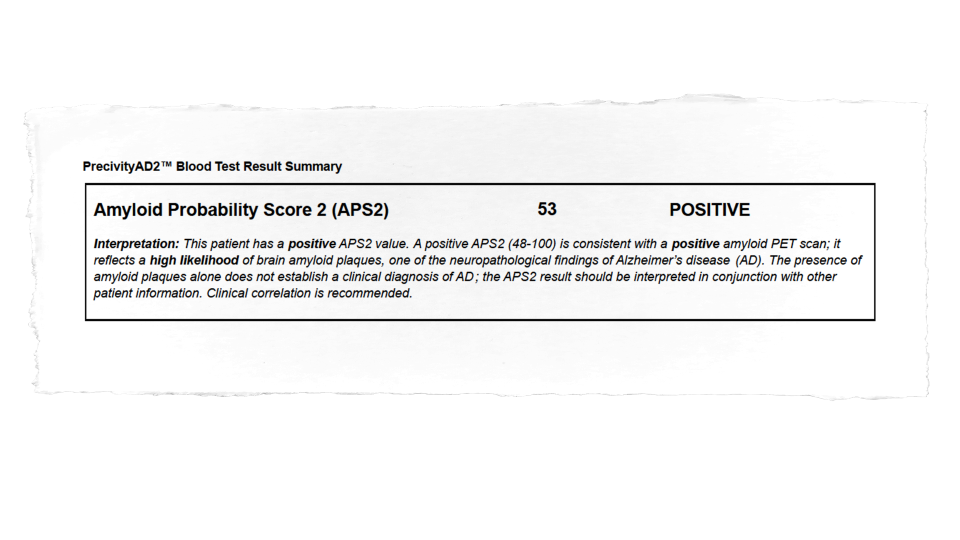
As part of the trial, Nicholls underwent a battery of tests, including a unique blood test that can track levels of amyloid, tau and other hallmark biomarkers for Alzheimer’s disease and other degenerative conditions. Deposits of amyloid can begin accumulating in the brain decades before symptoms begin, even in a person’s 30s and 40s.
“Simon’s first test came back with a score of 70. Anything over 58 was positive for amyloid in the brain,” Isaacson said. “The results backed up the amyloid PET scan Simon had taken in 2019, where I could see the plaque in his brain.”
10,000 steps a day: ‘I’m very consistent’
Nicholls needed to lose weight, so he began taking tirzepatide (the active ingredient in the medications Mounjaro and Zepbound), one of the newer injectable drugs that suppress appetite by stimulating hormones that control blood sugar levels.
At the same time, Nicholls was encouraged to step up his physical activity by incorporating strength training three times a week while adding 45 to 60 minutes a day of zone 2 exercise, in which you briskly walk, ruck, jog or cycle at 60% to 70% of your heart rate.
“I love going for a walk every morning at sunrise for an hour and a half with a podcast. I get in 10,000 steps or more every day. I’m very consistent,” Nicholls said. “I also do a very slow full-body workout with weights three times a week for an hour’s time.”
Avoiding sugar, artificial sweeteners, alcohol and ultraprocessed foods is a must, as is following a plant-based meal plan such as the Mediterranean diet.
“When I first saw Simon, he had a bit of a middle, like most guys in their 50s,” Isaacson said. “When I saw him at nine weeks, I did a double take. He was totally buff, ripped even.
“Within those nine weeks, he had lost 21 pounds, about 80% of that fat, and put on muscle, which was excellent,” Isaacson added. “I almost didn’t recognize him.”
The weight loss and increased muscle mass lowered Nicholls’ fasting blood sugar levels, ending his march toward diabetes, while some tweaks to his cholesterol medications further optimized his good and bad cholesterol numbers.
In August 2023, it was time to repeat the blood test for amyloid. By then, the company that administers the tests had added a measurement for tau, another key hallmark sign of Alzheimer’s, frontal lobe dementia and Lewy body disease.
“Simon’s amyloid probability score on the new APS2 test had dropped to 53, which was phenomenal,” Isaacson said. “But he was still positive, as anything between 48 and 100 is considered to reflect a high probability of amyloid brain plaques on a brain scan.”
‘Turn on the screws’
Now that the big concerns of cholesterol, insulin, diet, exercise and fat mass were addressed, it was time “to turn on the screws,” Isaacson said, with personalized recommendations based on Nicholls’ biology.
“We optimized Simon’s omega-3 fatty acid levels, which is especially important for people with APOE ε4, as they need more omega-3. We also added B complex vitamins to control elevated homocysteine in his blood,” Isaacson said. “However, we would not give B complex vitamins to anyone who did not have higher homocysteine levels.”
Elevated homocysteine, which is an amino acid used by the body to make protein, is a risk factor for brain atrophy, cognitive impairment and dementia. A September 2010 randomized controlled trial found that supplementation slowed brain atrophy in people with mild cognitive impairment.
In the meantime, Nicholls, an avid researcher who loves to read medical journals, was adding some interventions of his own.
“I have steam and sauna rooms in my home, I do a lot of that. I love it,” he said. “I’ve tried cold water plunges, and I have lists of things to do I get from podcasts, from walking to sleeping to gratitude to yoga to sleep routines.
“But there’s one thing I do that Dr. Isaacson doesn’t agree with: I get stem cell injections twice a year,” Nicholls added. “Sadly, I have arthritis in my hands, and that definitely feels better when I use stem cells, and I like to think they may be helping my brain, as well.”
There was one more big issue to tackle: Nicholls’ sleep, or lack of it, which studies have shown can hasten cognitive decline and Alzheimer’s.
With business around the world, Nicholls is a frequent flyer with “terrible sleep” due to jet lag and insomnia. “I’m also a worrier type of person,” he confessed.
Adding a sleep medication approved for insomnia helped, “but Simon really needs to tackle his sleep by improving his sleep hygiene with a more regular sleep schedule,” Isaacson said.
An unbelievable result
On Halloween 2023, the next APS2 score arrived. Amazingly, Nicholls had reduced the amount of amyloid and tau in his blood to 40: He was testing negative in blood for signs of Alzheimer’s.
Shocked and amazed, Isaacson remained skeptical. “I was very cautious. You know, promise not to overpromise. I needed to retest.”
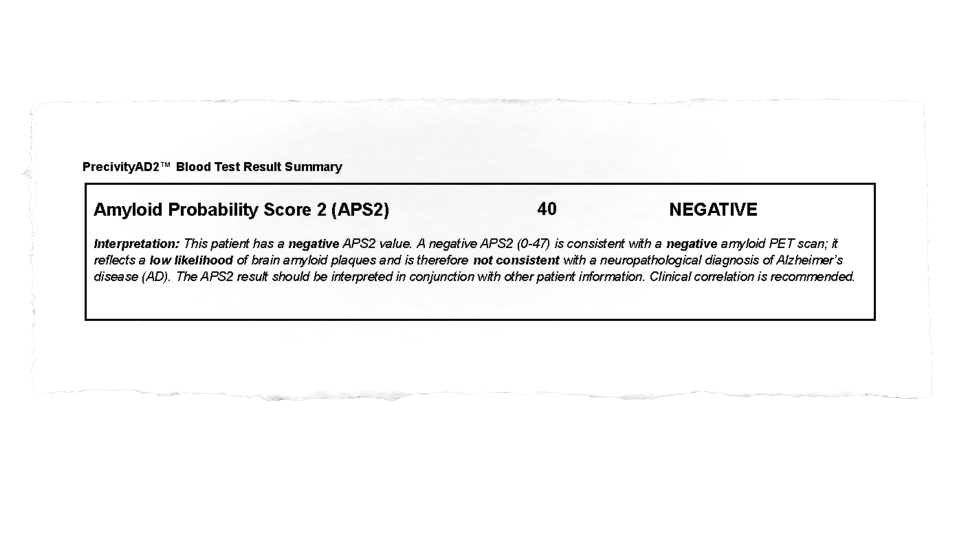
A few days before Christmas, the repeat test results arrived. When it too was a negative finding of 40, Isaacson decided to tell Nicholls in person.
“Dr. Isaacson drove all the way from Boca Raton to Miami excited, very happy,” Nicholls said. “We walked on a beach together, and we were ecstatic that we’d actually been able go from positive to negative for amyloid.”
Although Nicholls is ecstatic about the improvements, he’s also very humble about his efforts to improve his health.
“I’m really not all that compliant. To comply is just horrendously difficult, right? Of course I want to have a beer or a hamburger or something stupid. I love gummy bears and eating crappy food,” he said.
“It’s helped that I have some great doctors to help me, but to be honest, my biggest motivator are my children,” Nicholls added. “I’d love to see my sons get married and have their own kids, and to do that, I have to put in the work to stay the way I am now.”

Even lower amyloid levels and a larger hippocampus
It appears Nicholls is well on his way toward that goal. In March, his APS2 score had dropped to 25, an unbelievably low number.
Not only was Nicholls blood negative for amyloid and tau, the test suggested that his brain amyloid might be normal, with no distinguishable signs of the disease. The only way to definitively prove this, however, would be to repeat his amyloid PET scan, Isaacson said.
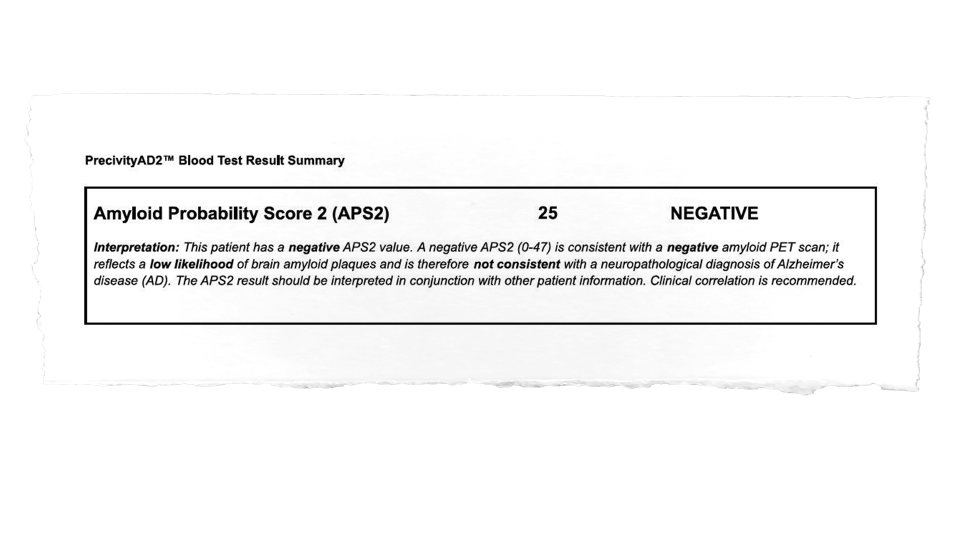
“What really drove his score down was the amyloid value,” Isaacson said. “It normalized at .101, which is like crazy good. That’s not matter for discussion; for amyloid, .1 or above is normal.”
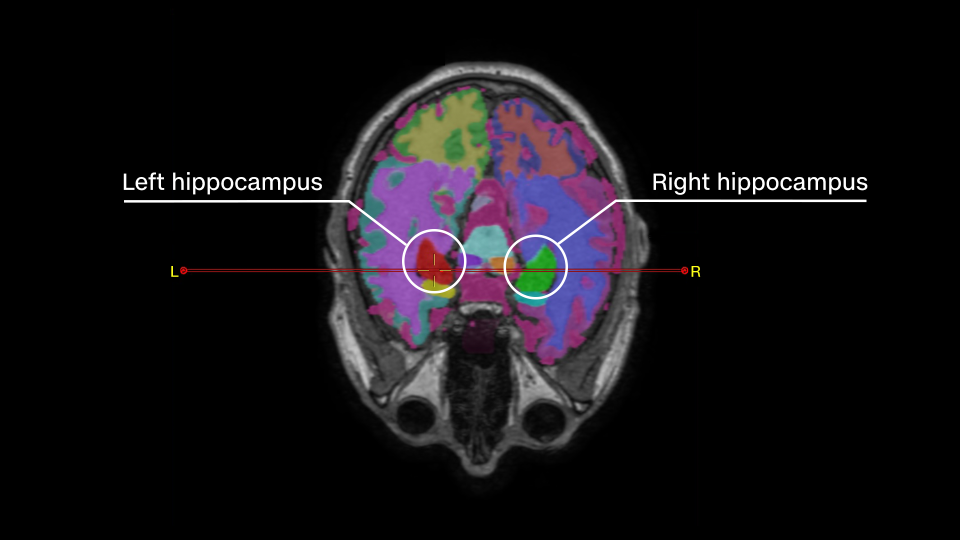
Even more startling: Brain volume scans showed that the hippocampus, the tiny seahorse-shaped organ responsible for memory, had actually grown in volume in Nicholls’ brain since he started the intervention.
In early Alzheimer’s stages, the hippocampus loses tissue rapidly and then atrophies as the disease progresses.
Despite these amazing outcomes, Isaacson remains cautious. After all, this is one person, and similar findings have not been been replicated in a larger, more controlled sample and published in a peer-reviewed journal.
“I don’t believe in the term ‘reverse’ because I don’t know what will happen if the person stops doing the intervention,” Isaacson said. “I also don’t know if the brain might normalize for a short period of time and then, five years later, catch up. Until I have more data, I don’t think that reverse is the right word.”
That doesn’t stop his wonder at the results and his gratitude to Nicholls for his continuing dedication to the study and the personalized interventions.
“I still can’t believe it. I’d seen this before, but only in people who are taking anti-amyloid medications,” Isaacson said. “When you work your entire career and are told by everyone, ‘It’s not possible to do this,’ and then you see it — well, I’m still humbled and amazed.”
Alzheimer’s and brain health resources
Want to learn more about brain health? Visit Isaacson’s free online course.
Consider joining Isaacson’s latest online clinical trial, designed to provide cognitive assessments and personalized advice via smartphones. People over 21 who meet certain criteria can sign up for the study at Retain Your Brain.
The National Institute on Aging currently supports nearly 500 active clinical trials on Alzheimer’s disease and related dementias. For information, go here.
The Alzheimer’s Association is looking for individuals living with Alzheimer’s, their caregivers and those without cognitive decline to volunteer for clinical trials.
For more CNN news and newsletters create an account at CNN.com


